A 26 year old lady with lower extremity weakness, emesis and severe hypokalemia. Overview
- Presenting Complaint
- Patient History
- Review of Systems
- Physical Examination
- Diagnostic Test
- Diagnostic Imaging
- Diagnosis and Management
- Discussion
26 year old lady with lower extremity weakness, emesis and severe hypokalemia and acne flare up
- History of presenting
- Past Medical/Social history
- Past surgical history
- Family history
- Current Medication
Recurrent admissions for weakness and low potassium.
negative for supplements or herbs.
not on any weight loss diet
no tobacco, alcohol, or drug use.
no occupational exposures
Her father died at 71 years from MI
sister - cutaneous lupus
Amitriptyline
dry mouth
unintentional weight loss of 12 pounds
Pelvic bony pains
General
Heent
Neck
Cardiovascular
Lungs
Abdomen
Extremities
Skin
Neurological Exam
- Bio Chemistry
- Pathology
- Microbiology
- Hematology
- Miscellaneous
Sodium: 137meq/L( normal 135-145 meq/L)
Potassium: 1.5meq/L (normal 3.5-5.0 meq/L)
Chloride: 115meq/L(normal 96-108 meq/L)
Bicarb: 15meq/L(normal 22-30 meq/L)
Magnesium: 2.2mg/dl ( normal 1.7 to 2.2 mg/dL )
Phos.: 2.5mg/dl ( normal 2.8 to 4.5 mg/dL)
Bun: 22 mg/dl ( normal 6-23 mg/dL)
Creat: 2.3 mg/dl ( normal 0.7 -1.3 mg/dL)
Liver Enzymes - SGOT/AST: 32U/L ( normal 1-35 )
SGPT/ ALT: 41U/L ( normal 1-45 )
GGT: 38U/L ( normal 8-38 )
Direct Bilirubin: 0.2mg/dl ( normal 0.1-0.3 )
Total Bilirubin: 1mg/dl ( normal 0.1 - 1.2 )
7.2: urine ph
no growth - urine culture
Hemoglobin: 12 g/dl
Hematocrit: 35
White Count: 5.7
Platelets: 175
Differential: WNL
Urine studies showed urine pH 7.2.
, high urine anion gap (UAG) of + 38,
urine osmolal gap of 60 mOsm/L,
potassium-to-creatinine ratio (K/Cr) of 20 mEq/g
- CT Scan
- Xray
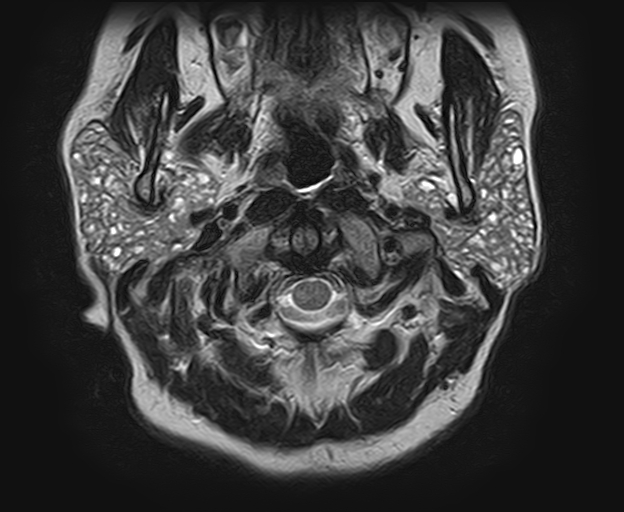
- MRI
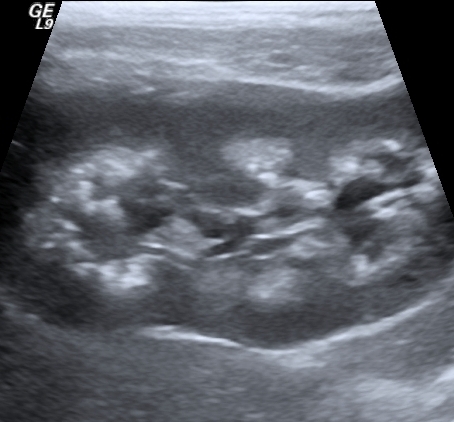
- Ultrasound
- Echo
- Endoscopic
- Miscellaneous
NOT APPLICABLE
diffuse demineralization: osteoporotic-like pattern
Case courtesy of Dr Mohammad Taghi Niknejad, <a href=”https://radiopaedia.org/”>Radiopaedia.org</a>. From the case <a href=”https://radiopaedia.org/cases/20086″>rID: 20086</a>
salt and pepper appearance, due to a combination of punctate regions of calcification (pepper) and fatty replacement (salt)
Case courtesy of Dr Ammar Haouimi, <a href=”https://radiopaedia.org/”>Radiopaedia.org</a>. From the case <a href=”https://radiopaedia.org/cases/67792″>rID: 67792</a>
medullary deposition of calcium salts in the parenchyma of the kidney
Case courtesy of Dr Hani Salam, <a href=”https://radiopaedia.org/”>Radiopaedia.org</a>. From the case <a href=”https://radiopaedia.org/cases/9899″>rID: 9899</a>
NOT APPLICABLE
NOT APPLICABLE
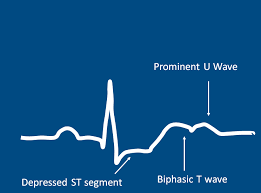
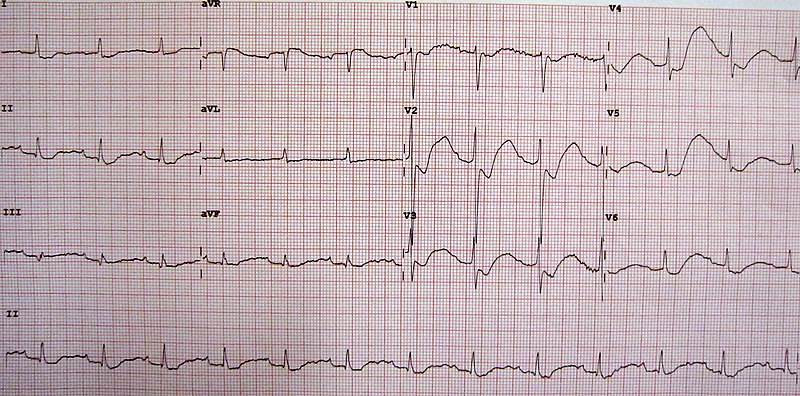
EKG
ST segment depression, inverted T waves, large U waves, and a slightly prolonged PR interval.
HYPOKALEMIA QUIZ
- The diagnosis of RTA requires measurement of the urine pH and estimation of urinary ammonium excretion. The urine pH is persistently 5.5 or higher in patients with distal RTA. ( pH was 7.2 in this case) . The UAG is sodium plus potassium concentrations and the urine chloride concentration in the urine is a indirect estimate of the urinary NH4 excretion..A negative UAG that is less than -20 is usually indicative of increased NH4 excretion UAG is generally between -20 and -50 mEq/L in patients with metabolic acidosis generated by diarrhea. A positive UAG > 20 is suggestive of low or normal NH4 excretion. In distal RTA patients have a positive UAG ( as in our patient )
An alternative method to estimate renal acid excretion ability is use of Urine Osmolal gap. The relationship between the UOG and NH4 excretion is not interfered by certain conditions which can disrupt the relationship between urine NH4 and the UAG. The UOG is calculated as the mathematical difference between the directly measured urine osmolality and the calculated urine osmolality. Calculated urine osmolality (mosmol/kg) = (2 x [Na + K]) + [urea nitrogen in mg/dL]/2.8 + [glucose in mg/dL]/18.•In chronic metabolic acidosis NH4 excretion, is increased to > 200 to 300 mEq/day , a value below 75 mEq/L in a patient with chronic metabolic acidosis suggests impairment in NH4 excretion. •When the UOG exceeds 400 mosmol/kg, it is likely that the urine NH4 concentration > 200 mEq/L or greater as commonly seen with hyperchloremic metabolic acidosis due chronic diarrhea . A UOG of less than 150 mosmol/kg in a patient with chronic metabolic acidosis suggests that NH4 excretion is impaired. Because NH4 excretion is reduced in patients with distal RTA, a low UOG is consistent with renal tubular defects.
- . Although vomiting can cause fluid loss directly from gastrointestinal tract, potassium depletion in this setting is primarily due to increased urinary losses from the fact that concentration of potassium in gastric secretions is only 5 to 10 mEq/L. Loss of gastric acid induces metabolic alkalosis and high plasma bicarbonate level. Water and sodium bicarbonate are transported to the distal potassium secretory site. In addition, hypovolemia from vomiting induces increase in aldosterone release. These 2 effects increase renal potassium loss in the urine and cause hypokalemia.
- The urine pH in proximal RTA will be appropriately 5.3 or less if the filtered bicarbonate load is reduced and can be completely reabsorbed, which most often occurs in untreated patients(patient in this case not on chronic treatment)
- Type 4 renal tubular acidosis and appears to be due primarily to decreased urinary ammonium excretion and presents typically with hyperchloremic acidosis) unless there is concurrent renal insufficiency. Reduced aldosterone secretion or aldosterone resistance leads to hyperkalemia and a mild hyperchloremic metabolic acidosis
RENAL FAILURE QUIZ
Sjögren’s syndrome is an autoimmune condition which typically involves lymphocytic infiltration of the salivary, parotid and lacrimal glands, resulting in the characteristic symptoms of xerosis (dry eyes) and xerostomia (dry mouth). This immune process can also affect non-exocrine organs, such as the skin, lungs, gastrointestinal tract and the kidneys. Tubulointerstitial inflammation in the form of TIN is the most common renal manifestation of Sjögren’s syndrome. It can also lead to nephrocalcinosis and renal calculi. Histological findings in RTA secondary to Sjögren’s are typically described as diffuse lymphocytic infiltration in the renal interstitial tissues, interspersed with plasma cells. Depending on the segment of the nephron impacted by lymphocytic infiltration, TIN has been shown to manifest as hypokalemia, acidosis, RTA (predominantly distal and rarely proximal), Gitelman syndrome, Fanconi syndrome and diabetes insipidus Similarly, it can



interesting case
good case quizzes