Correct Answer is A
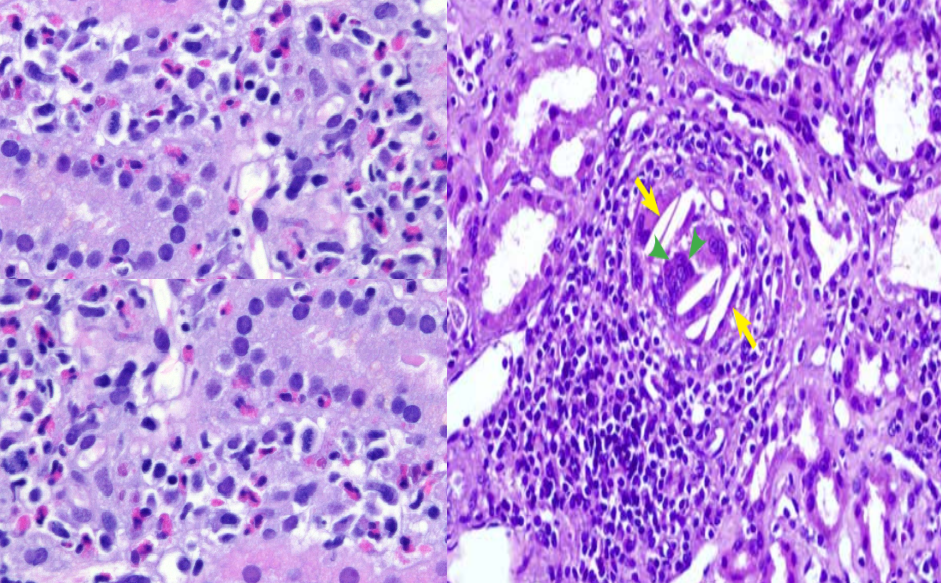
A.Warfarin has been shown to cause AKI by multiple different mechanisms including atheroembolism, glomerular hemorrhage, tubular obstruction by RBC casts, and acute interstitial nephritis. It has been hypothesized that warfarin may dissolve the fibrin clot or impair the fibrin thrombus formation over the ulcerated atherosclerotic plaque (patient has preexisting AAA), leading to destabilization of the atheroma and subsequent embolization. The cholesterol crystals can trigger an inflammatory cascade leading to constitutional symptoms of fever, fatigue, anorexia, weight loss, and myalgias. His Renal Biopsy shows focal interstitial infiltrate consisting of lymphocytes, plasma cells, and eosinophils, intimal fibrosis noticed in interlobular arteries. The classic lesion in AERD is the cholesterol emboli causing blockage of arcuate/ interlobular arteries/glomerular capillaries. This lesion is recognized as a characteristic biconvex, needle-shaped clefts appearing as “empty space” in the center (SEE IMAGE) caused due to dissolution of the crystals using routine histologic preparation. A birefringent character of the cholesterol crystals under polarized light, can be demonstrated by using liquid nitrogen to snap freeze the specimen. skin manifestations of Ather emboli include livedo reticularis, blue toe/purple toe syndrome. Intestinal ischemia presenting as abdominal pain and neurological deficits from spinal emboli can occur. Eosinophilia, elevated ESR, CRP and hypocomplementemia can also be present. Hollenhorst plaques on fundoscopy due to retinal embolization can occur. Renal involvement is seen in more than 50% of the cases, with progression to dialysis in 28-61%, and 1 year mortality rate up to 83%. The rationale behind use of steroids in AERD is not clear, but a decrease in reactive inflammation from activation of the complement (hypocomplementemia often present in AERD) in many patients suggests a possible role for inflammation in pathogenesis of AERD and in its occasional response to steroid therapy.
B.WRN- warfarin related nephropathy is defined as an acute increase in serum creatinine of >0.3 mg/dl within 1 week of an INR >3.0. The cause of renal damage is glomerular hemorrhage and tubular RBC casts causing obstruction and inflammatory and oxidative damage to the tubular epithelial cells. In various studies, the average INR among patients with ARN was in the mid to upper 4s. Microscopic hematuria is common though absence of hematuria does not exclude a possible diagnosis of ARN. Renal Biopsy shows congested glomerulus with red blood cells in the capillary vessels. there is diffuse tubular damage with large and occlusive RBC casts in the tubules. IF is negative and glomerular architecture is maintained with absence of endocapillary or extra capillary glomerulonephritis related changes.
C. CIN – contrast induced nephropathy – creatinine rises within 24 to 48 hours after the iodinated contrast exposure and starts to decline toward baseline within three to seven days of the exposure to contrast. The timeline of creatinine rise does not suggest CIN. patient left hospital with his previous baseline creatinine after contrast exposure. UA can be expected to show acute tubular necrosis (ATN), including muddy brown granular and epithelial cell casts and free renal tubular epithelial cells for this degree of AKI.
D. Warfarin induced AIN – Although response to steroids may suggest AIN, classically, patients with drug-induced AIN present with signs of an allergic-type reaction, including rash, fever, and eosinophilia, although these may be absent – renal biopsy can present with interstitial infiltrate consisting of lymphocytes, plasma cells, and eosinophils, however intimal fibrosis noticed in interlobular arteries with cholesterol clefts is not typical of AIN.
REFERENCES
Warfarin related acute kidney injury: A case report (nih.gov)
Atheroembolic Renal Disease | American Society of Nephrology (asnjournals.org)