Answer is D
Treatment of RVT in a patient with nephrotic syndrome and AKI includes local thrombolytic therapy with percutaneous catheter thrombectomy when there is a large clot burden (as in in this patient- clot extending to IVC), bilateral RVT, or a solitary kidney. Direct oral anticoagulants (DOACs) have limited data for use in patients with nephrotic syndrome and can be considered in patients with side effects or failure of therapeutic effects from warfarin/LMW heparin, if the patient is unwilling to take low-molecular-weight heparin/coumadin. anticoagulation is continued until remission of nephrotic syndrome or when a serum albumin above 3.0 g/dL is achieved. Prophylactic anticoagulation recommendations for membranous nephropathy related nephrotic syndrome involves with assessment of risk factors for bleeding (HAS-BLED bleeding risk score)-
A) anticoagulation-associated bleeding risk is high, or the serum albumin level is ≥3.0 g/dL, do not administer prophylactic anticoagulation.
B) If the anticoagulation-associated bleeding risk is low and the serum albumin level is level is ≥3.0 g/dL, prophylactic anticoagulation with low-molecular-weight heparin or warfarin.
C)If the anticoagulation-associated bleeding risk is intermediate and the serum albumin level is less than 2.0 g/dL, administer prophylactic anticoagulation with low-molecular-weight heparin or warfarin.
D) If the anticoagulation-associated bleeding risk is intermediate and the serum albumin level is between 2.0 and 2.9 g/dL, the decision to administer prophylactic anticoagulation should be made on a case-by-case basis.
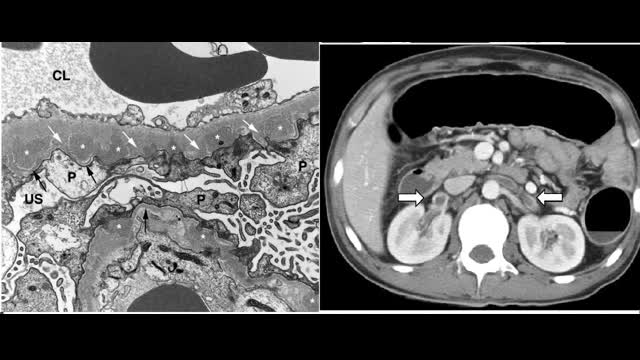
One needs to suspect RVT in any patient with membranous nephropathy presenting with flank pain and worsening proteinuria / AKI. Complications of severe nephrotic syndrome (proteinuria above 3.5 g/d and serum albumin less than 3 g/dl) venous thrombosis such as RVT/DVT /PE/ cerebral venous thrombosis and also Arterial thrombotic events. Prevalence of RVT is higher with nephrotic syndrome due to membranous nephropathy compared to other nephrotic diseases (20%–60%) tends to occur early in the course of the disease. Reasons for RVT in nephrotic syndrome is due to low levels of antithrombin III, plasminogen, and protein C/S from proteinuria wasting. concentration of blood in the post glomerular circulation, Hyperfibrinogenemia, high molecular weight fibrinogen moieties, increased platelet activation, and inhibition of plasminogen activation contribute to hypercoagulability. A serum albumin less than 2.0 g/dl appears to be associated with increased risk for venous thrombosis and is a surrogate marker for hypercoagulability. Differential diagnosis for etiology of RVT includes other hypercoagulable states as well as renal cell carcinoma which can with RVT. diagnosis of RVT is best done by Selective renal venography (gold standard;) – noninvasive tests such CT angiography with venous phase imaging and magnetic resonance venography are also have good sensitivity/specificity Doppler ultrasonography does not have good sensitivity and specificity.
REFERENCES
Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome – PubMed (nih.gov)
Kidney Int 1985; 28:42
Thrombosis and hemostasis in renal disease – PubMed (nih.gov)Rabelink TJ, Zwaginga JJ, Koomans HA, Sixma JJ. Thrombosis and hemostasis in renal disease. Kidney Int 1994; 46:287.
Llach
Complications of the nephrotic syndrome and their treatment – PubMed (nih.gov)Crew RJ, Radhakrishnan J, Appel G. Complications of the nephrotic syndrome and their treatment. Clin Nephrol 2004; 62:245.