Correct answer is D
Salicylic acid (HSal) is a weak acid and has an equilibrium reaction- H+ + Sal- <—> HSal. If the systemic pH is decreased (more H+ ions), the equation will move to the right. The resulting rise in plasma HSal concentration will allow HSal to diffuse from extracellular fluid into the CNS down a favorable concentration gradient worsening neurotoxicity. The increase in the CNS salicylic acid concentration( HSal) then causes the equation to move to the left in the brain cell where it will be trapped as Sal-. The subsequent lowering of intracellular salicylic acid HSal concentration in the CNS promotes further HSal drug movement from extracellular fluid into the CNS further increasing CNS toxicity in a self-perpetuating cycle. Diamox (Acetazolamide) is a carbonic anhydrase inhibitor that alkalinizes the urine by reducing bicarbonate reabsorption in proximal tubule. It is contraindicated in the standard management of salicylate poisoning. While it increases salicylate excretion by increasing urine alkalization, the resultant bicarbonate loss from plasma lowers the arterial pH, promoting salicylate movement into the CNS and causes worsening salicylate neurotoxicity.
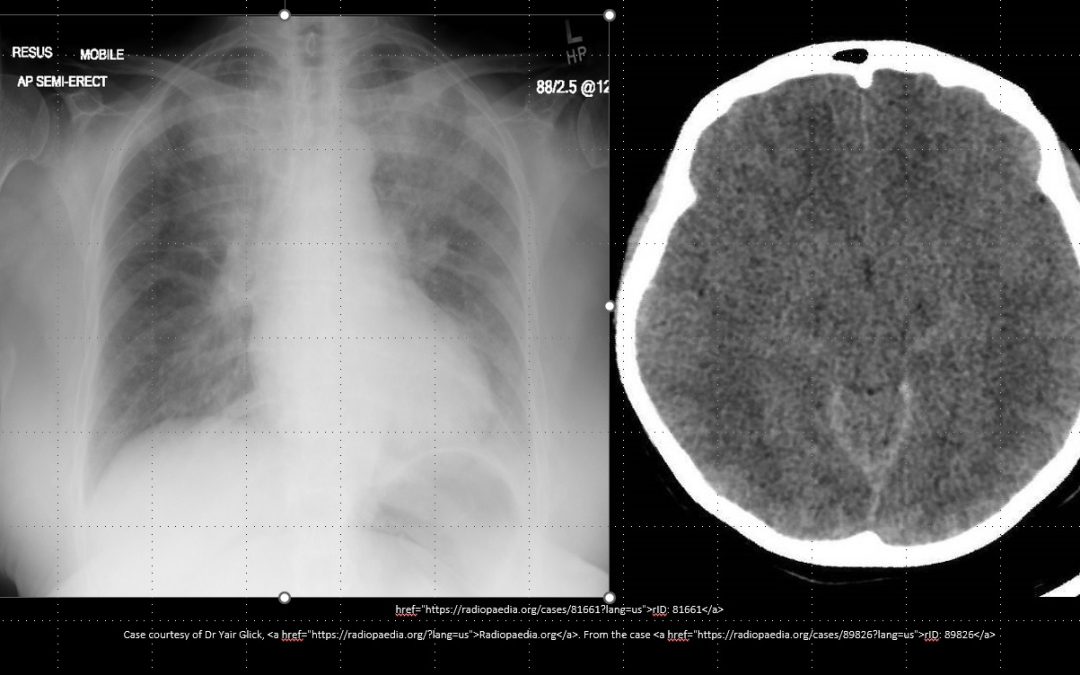
Indications for hemodialysis in salicylate poisoning include worsening clinical progress despite aggressive supportive care with following features- acute respiratory failure with pulm edema, AMS with cerebral edema(as seen in the MRI brain showing absence of sulcal markings and poor differentiation of white and gray matter), significant renal failure impairing salicylate elimination( Cr >1.5-2.0), high salicylate concentration of 90 mg/dL(without renal failure) or 80 mg/dL(with renal failure), fluid overload that prevents the administration of sodium bicarbonate, or IV normal saline and severe acidemia with a systemic pH ≤7.20.
Continuous renal replacement therapy (CRRT) is NOT equivalent to hemodialysis when treating the salicylate poisoning due to high level of Salicylate clearance using hemodialysis when compared to CRRT. Hemodialysis is also more effective in correcting the acid-base or electrolyte abnormalities associated with severe salicylate poisoning. CRRT is inferior to hemodialysis when renal replacement therapy is indicated in salicylate poisoning.
Salicylate poisoning can decrease CNS glucose levels despite a normal serum glucose. It is recommendd to maintain the patient’s serum glucose in the high normal range (approximately 80 to 120 mg/dL). IV boluses of dextrose (50 to 100 mL of 50 percent dextrose) can be used in patients with altered mental status with frequent monitoring of fingerstick glucose concentration every one to two hours, until the signs of severe toxicity resolve. Thus, supplemental glucose is recommended for patients with encephalopathy irrespective of serum glucose concentration.
Aspirin acts on the medullary respiratory center to increase Minute ventilation (Resp rate x tidal volume Vt = MV). The resulting respiratory alkalosis prevents the entry of salicylate into the CNS by trapping the salicylate anions in the blood. It is difficult to replicate a similar high minute ventilation with mechanical ventilation in patients with salicylate poisoning. The brief apnea period during resp muscle paralysis induced at the time of intubation can cause respiratory acidosis protonating salicylate anions to uncharged salicylic acid, which can enter to CNS by crossing the blood-brain barrier and promote CNS toxicity. Intubation should be reserved for those patients with severe hypoventilation. In this case, patient still has high resp rate, low pc02 on blood gas suggesting that he is not at risk of imminent primary respiratory failure at this time. He will be at higher risk of superimposed respiratory acidosis on top of metabolic acidosis during attempts to intubate, which can worsen his CNS toxicity.
References
.