CORRECT ANSWER IS D
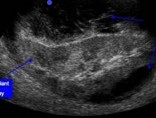
Patient developed Page kidney due to external compression of renal parenchyma following ESWL resulting in AKI. The subcapsular space of kidney is a potential space that causes compression of the kidneys after minimal leakage of blood & manifests as hypertension and worsening of renal function. Most common reasons are Hematomas, masses or fluid collection, that lead to compression of the kidney and activation of the renin-angiotensin-aldosterone system, resulting in systemic hypertension and then renal failure. Sub capsular bleeding is the one of the most frequent etiology for Page kidney and commonly complicates renal biopsy and electroshock wave lithotripsy (ESWL). Doppler ultrasound shows elevated resistive index(RI). High RI values in a transplanted kidney doppler ultrasound is nonspecific and can also be seen in renal vein thrombosis, ureteral obstruction, acute rejection, pyelonephritis, acute tubular necrosis and may be an artifact secondary to manual compression by the US transducer. Treatment of the transplant Page kidney phenomenon needs to be aggressive with evacuation of the subcapsular bleeding to ensure optimal viability of the allograft.
Lymphocele is one of the most common complications after kidney transplantation and occurs usually between 2 weeks to 6 months after transplantation with a peak incidence at 6 weeks. Rarely, in some studies, lymphocele has been reported 3.7 years after transplantation. This patient is 4 years post-transplant and had normal renal function prior to most recent AKI, making Lymphocele as a less likely cause for AKI. Lymphocele can cause pressure on the kidney transplant, ureter, bladder, and adjacent vessels with deterioration of graft function, ipsilateral leg edema, and external iliac vein thrombosis. They occur secondary to transection of lymphatic vessels during dissection of the iliac vasculature and can cause mass effect compression of the transplanted kidney, ureter, or vessels, compromising allograft function. Interventions for postoperative lymphocele include ethiodized oil lymphangiography, percutaneous aspiration, laparoscopic, or open peritoneal fenestration.
Renal Biopsy to rule out rejection is not right choice. Rejection is less likely despite high resistive indices on renal doppler. Most episodes of acute rejection occur around 6 months post-transplant with increased risk early after surgery. Rejection beyond 2 months is typically from noncompliance or overaggressive reduction in immunosuppression. There is no history of noncompliance and IS regimen changes. There are alternative explanations and radiology findings to explain his AKI and so renal biopsy should not be done at this time. Anti GBM disease less likely despite CXR findings as serology negative and clinical history is not suggestive.
Imaging study revealed a stone partially blocking the ureter of transplant kidney during the second episode of AKI. There is no hydronephrosis making obstructive uropathy from stone disease as less likely cause for recurrent AKI. Urgent Urology referral is not right choice at this time.
REFERENCES
Lymphatic disorders after renal transplantation: new insights for an old complication (nih.gov)
Page kidney as a complication after a shock wave lithotripsy: a case report (nih.gov)
https://openjournals.utoledo.edu/index.php/translation/article/download/420/288/1871